高血压和糖尿病是女性在妊娠期内常见的两类重要的代谢性疾病。在全球范围内,特别是低收入和中等收入国家,这两类疾病仍是造成孕产妇死亡的主要原因。经过多年的干预措施,妊娠期代谢性疾病的患病率有所下降,但在许多国家,妊娠期代谢性疾病的患病率在过去二十年中急剧增加了30%以上。
近日,清华大学万科公共卫生与健康学院唐昆副教授及其团队与多伦多大学全球儿童健康研究中心(Centre for Global Child Health, SickKids Hospital, University of Toronto)合作以共同第一作者身份,在《自然综述:内分泌学》(Nature Reviews Endocrinology)发表了题为《全球视角下孕产妇妊娠期高血压及糖尿病》(A global view of hypertensive disorders and diabetes mellitus during pregnancy)的系统综述研究。
该研究系统性地回顾了孕产妇妊娠期高血压和糖尿病的全球疾病负担和风险因素,并重点关注高收入国家和中低收入国家之间的差异。此外,该研究致力于提供公共卫生干预的政策建议,提倡以一种有效且具有高成本效益的方式促进妊娠期代谢性疾病死亡率和发病率的降低。
全球妊娠期高血压在育龄妇女中的平均患病率为116.4/10万,大约9-25%的孕妇会在妊娠期受到糖尿病及其并发症的影响。两种疾病的患病情况在全球区域层面呈现明显的不平等现象。在高收入国家和中低收入国家的疾病负担也呈现出显著的差异。


2019年妊娠期高血压疾病的全球流行情况
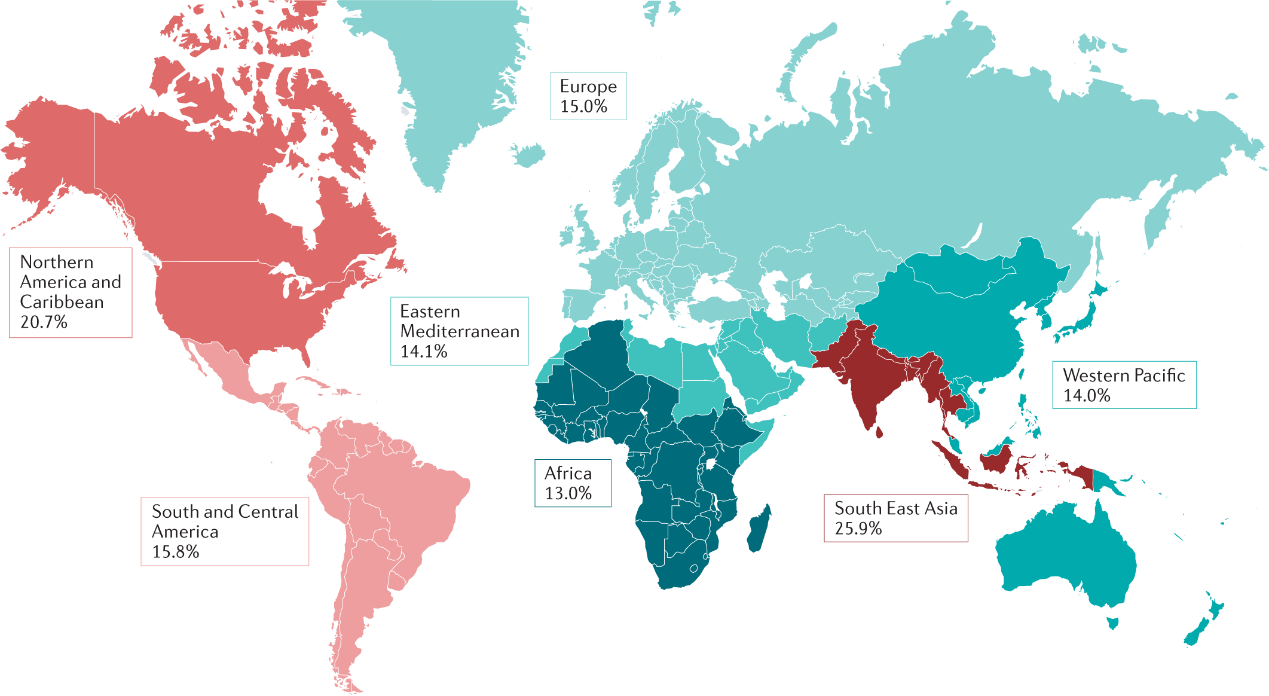
2021年妊娠期糖尿病的全球流行情况
为了进一步说明在国家层面上妊娠期高血压负担的潜在差异,该研究将妊娠期高血压的疾病负担分别按“国家和社会人口指数”(SDI)和“人类发展指数”(HDI)进行分层。研究发现,可持续发展指数和人类发展指数较低的国家一般有更大的妊娠期高血压疾病负担,表现为较高的患病率、伤残调整寿命年(DALYs)和归因死亡率。

2019年各国家和地区妊娠期高血压患病率与社会人口指数和人类发展指数的关系
两类疾病具有很多共同的风险因素,包括是否为高龄产妇、超重/肥胖、营养状况、怀孕前和/或怀孕期间的饮食模式、遗传因素和疾病史等。此外,种族、民族、社会经济和环境等因素也被证明与两类疾病有显著的相关性。
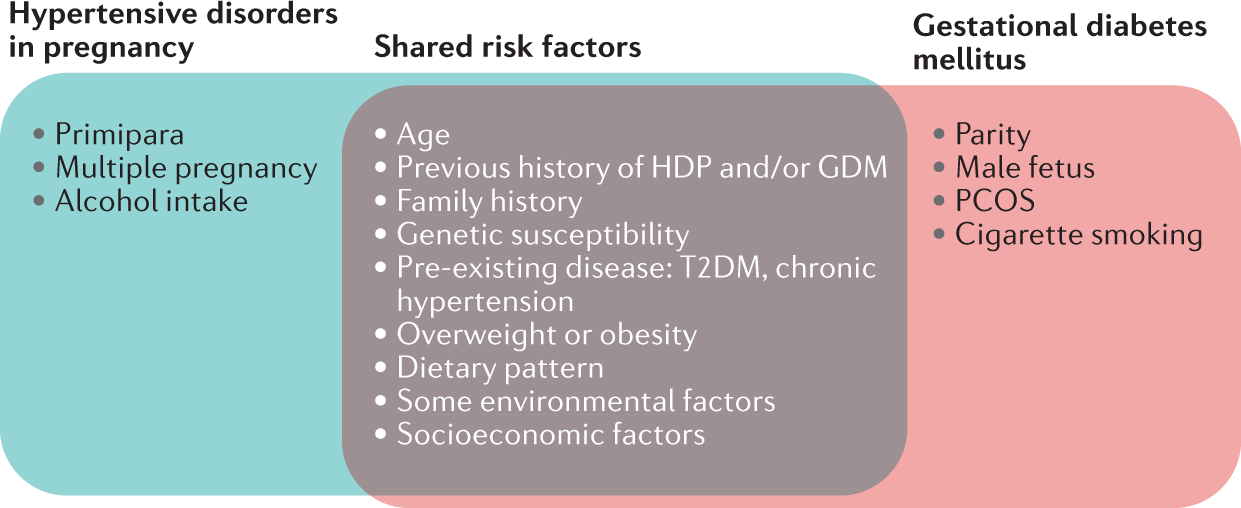
孕产妇心脏代谢障碍的主要危险因素
考虑到孕产妇代谢性疾病带来的巨大疾病负担,该研究整理和归纳了各国研究人员近几十年来探索出来的有效的临床治疗、疾病预防和管理、以及公共卫生干预手段。这些干预方法不仅可以改善妊娠期相关疾病的结局和预后,更可以改善患有代谢疾病的母亲及其子代的长期健康结局。
原文摘要
Two important maternal cardiometabolic disorders (CMDs), hypertensive disorders and diabetes in pregnancy, share many similarities. Although a global consensus has not been reached about the diagnostic criteria for maternal CMDs, making it challenging to assess differences in their disease burden between countries and areas. It has been revealed that, for both diseases, there is an unevenly distributed disease burden for regions and countries with a low- or middle-income, or with lower sociodemographic and human development indexes. In addition to many common clinical, demographic and behavioral risk factors, the development and clinical consequences of maternal CMDs were significantly influenced by social determinants of health such as systemic marginalization. Although there is novel progress in the early screening and management of maternal CMDs, their accuracy and long-term effects are still under investigation. In addition to pharmacological therapies and lifestyle modifications at the individual level, a multilevel approach in conjunction with multisector partnership should be adopted to tackle the public health issues and health inequity resulting from maternal CMDs. The current coronavirus disease 2019 (COVID-19) pandemic has disrupted health service delivery, with women with maternal CMDs being particularly vulnerable to this public health crisis.