肥胖、高血压、高血糖及血脂异常等常见代谢紊乱症状与饮食锻炼等个人生活习惯息息相关,除此之外,我们居住的环境是否也会对此带来影响呢?以及同时暴露的多种环境因素之间是否存在相互作用?

图1. 居住环境是否影响肥胖的患病风险
得益于遥感和地理信息技术的发展,如今我们可以利用卫星数据衡量个人居住地数百米范围内的多种环境暴露如绿地和空气污染水平,从而分析其与健康的关联。5月4日,清华大学万科公共卫生与健康学院副教授纪思翰(John Ji)课题组及其合作者在BMC Public Health 上发表的一项研究,Air Pollution, Residential Greenness, and Metabolic Dysfunction Biomarkers: Analyses in the Chinese Longitudinal Healthy Longevity Survey,分别分析了居住环境绿化、空气污染与代谢综合征(MetS)及其组成 (腹型肥胖、高血压、高血糖及血脂异常)之间的关联,并进一步探索了绿地和空气污染之间的交互作用。

图2 BMC Public Health官网发布截图
本研究的研究对象是老年健康生物标志物队列研究的中国八个长寿县区65岁-112岁的老年人。调查地区城镇和农村PM2.5水平相当,农村绿地(归一化植被指数NDVI)略高于城镇,通过将问卷调查数据、居住地信息和实验室检查指标相结合,研究发现PM2.5会增加代谢综合征、腹型肥胖、空腹血糖升高和高密度脂蛋白胆固醇降低的发生比,而且亚组分析显示这些关联只在农村地区具有显著的统计学意义,在城镇地区则不显著,而绿地与较低的腹型肥胖的关联仅在 PM2.5低的地区显著,在PM2.5高的地区则不显著。
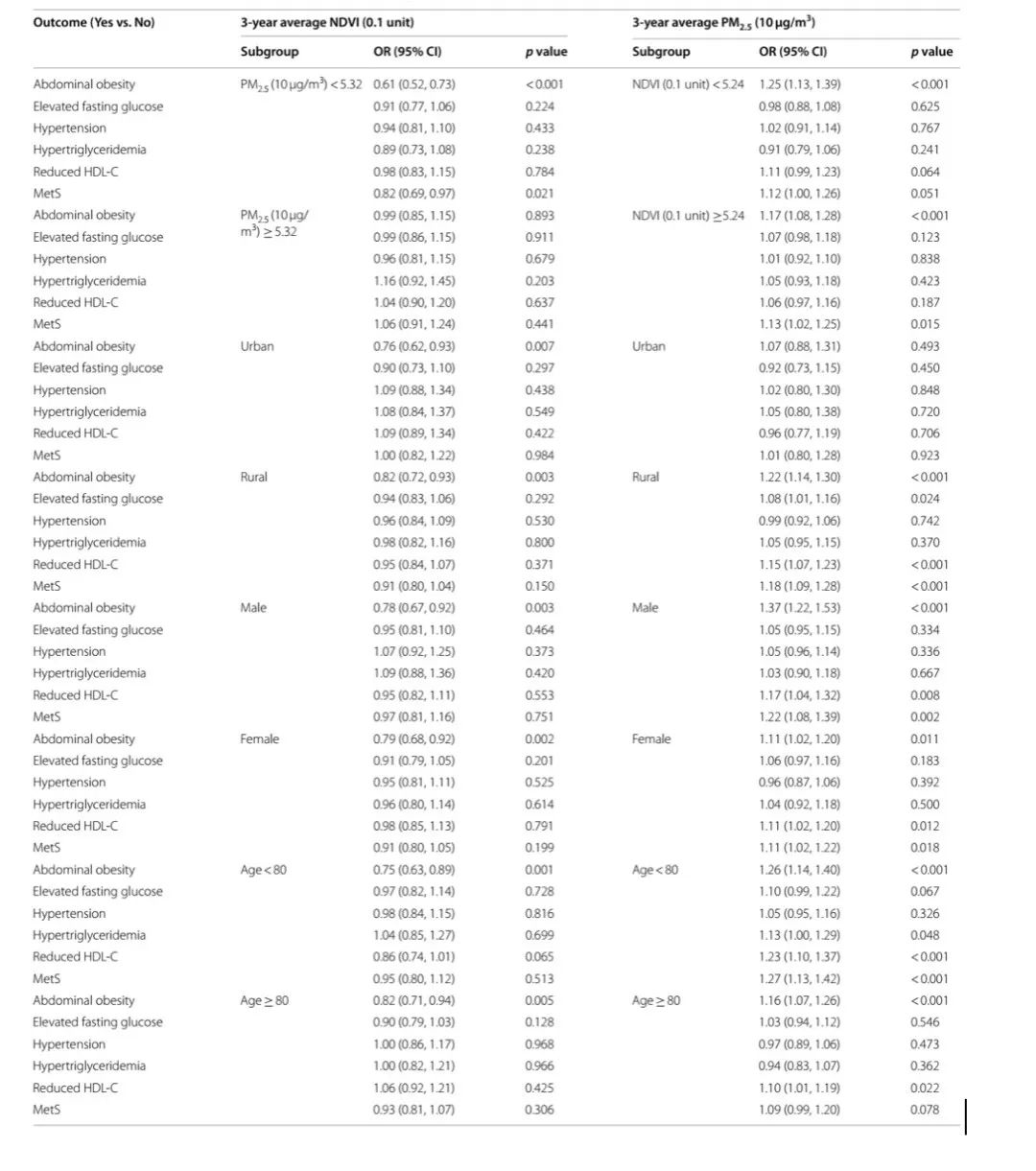
表1. 绿地、空气污染与代谢综合征及其组成在PM2.5、NDVI、年龄、性别和居住地各亚组中的相关性
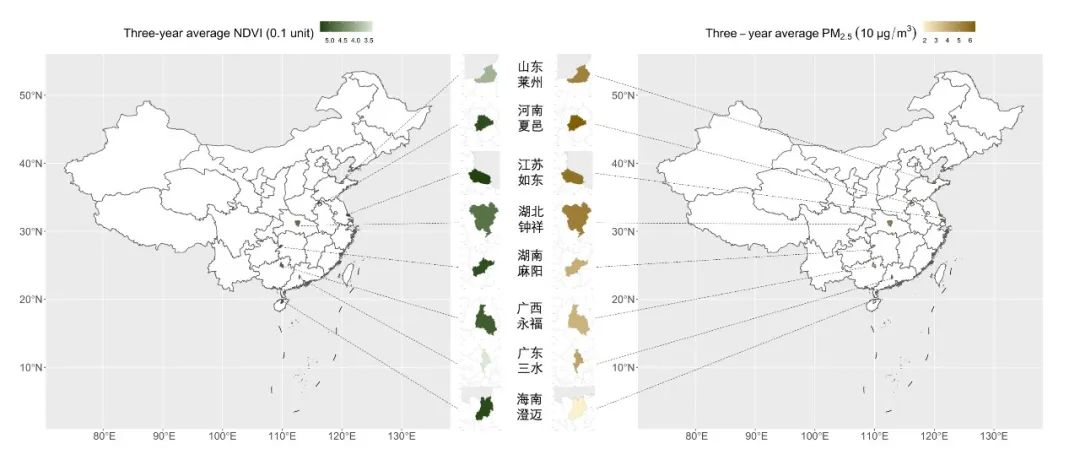
图3. 研究调查八个长寿地区NDVI及PM2.5的基线年均水平
代谢综合征是疾病和死亡的重要危险因素,这项研究利用中国长寿老年人队列,为绿地和空气污染共同影响人体代谢增加了新的证据,强调了在健康城市和健康村镇的建设中减轻农村地区空气污染和增强城镇地区绿地规划的重要性,提示腹型肥胖等代谢紊乱不仅可通过个人生活方式的改变来预防,重要的还有我们的居住环境,其规划改善影响人群更大,从而或可带来较大的健康收益。
Background:
We hypothesize higher air pollution and fewer greenness exposures jointly contribute to metabolic syndrome (MetS), as mechanisms on cardiometabolic mortality.
Methods:
We studied the samples in the Chinese Longitudinal Healthy Longevity Survey. We included 1755 participants in 2012, among which 1073 were followed up in 2014 and 561 in 2017. We used cross-sectional analysis for baseline data and the generalized estimating equations (GEE) model in a longitudinal analysis. We examined the independent and interactive effects of fine particulate matter (PM2.5) and Normalized Difference Vegetation Index (NDVI) on MetS. Adjustment covariates included biomarker measurement year, baseline age, sex, ethnicity, education, marriage, residence, exercise, smoking, alcohol drinking, and GDP per capita.
Results:
At baseline, the average age of participants was 85.6 (SD: 12.2; range: 65–112). Greenness was slightly higher in rural areas than urban areas (NDVI mean: 0.496 vs. 0.444; range: 0.151–0.698 vs. 0.133–0.644). Ambient air pollution was similar between rural and urban areas (PM2.5 mean: 49.0 vs. 49.1; range: 16.2–65.3 vs. 18.3–64.2). Both the cross-sectional and longitudinal analysis showed positive associations of PM2.5 with prevalent abdominal obesity (AO) and MetS, and a negative association of NDVI with prevalent AO. In the longitudinal data, the odds ratio (OR, 95% confidence interval-CI) of PM2.5 (per 10 μg/m3 increase) were 1.19 (1.12, 1.27), 1.16 (1.08, 1.24), and 1.14 (1.07, 1.21) for AO, MetS and reduced high-density lipoprotein cholesterol (HDL-C), respectively. NDVI (per 0.1 unit increase) was associated with lower AO prevalence [OR (95% CI): 0.79 (0.71, 0.88)], but not significantly associated with MetS [OR (95% CI): 0.93 (0.84, 1.04)]. PM2.5 and NDVI had a statistically significant interaction on AO prevalence (pinteraction: 0.025). The association between PM2.5 and MetS, AO, elevated fasting glucose and reduced HDL-C were only significant in rural areas, not in urban areas. The association between NDVI and AO was only significant in areas with low PM2.5, not under high PM2.5.
Conclusions:
We found air pollution and greenness had independent and interactive effect on MetS components, which may ultimately manifest in pre-mature mortality. These study findings call for green space planning in urban areas.
获取全文
扫码或点击“阅读原文”获取文章原文